April 11th, 2023 7:00am
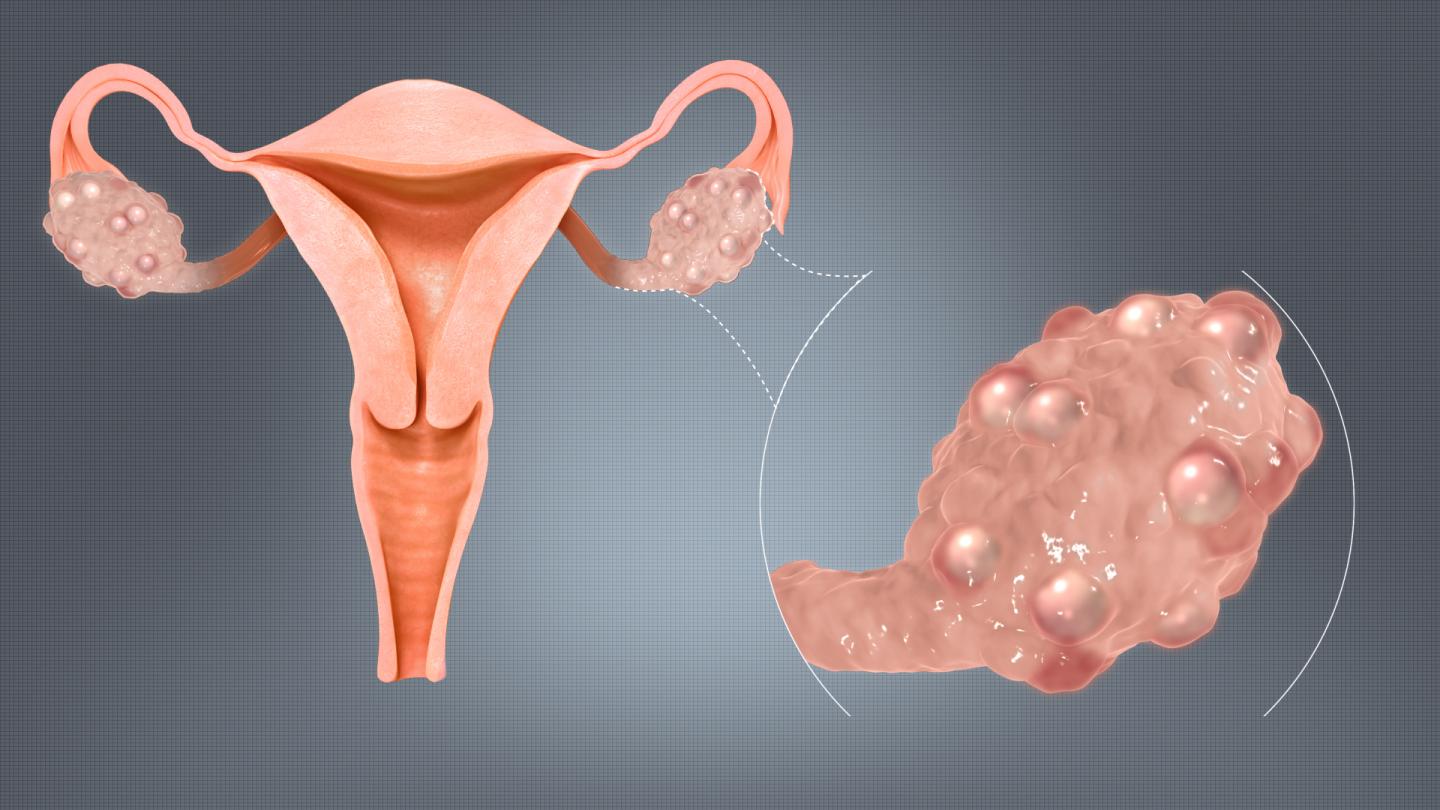
Polycystic ovarian syndrome (PCOS) is a hormonal disorder that is highly connected to insulin resistance and blood sugar imbalance. Up to 70% of women with PCOS have some level of insulin resistance that plays a role in their condition, regardless of weight or size. This insulin resistance puts people with PCOS at an increased risk for type II diabetes and metabolic syndrome.
Women with PCOS typically have high levels of testosterone and other hormonal imbalances creating symptoms such as hair growth, irritability, mood swings, acne, irregular or absent periods, heavy periods, headaches, depression, hair thinning, and infertility. Insulin resistance can play back into these hormonal imbalances by pushing testosterone production higher. Because blood sugar dysregulation is tied so closely to the hormonal imbalances in PCOS it’s important to consider blood sugar regulation as part of the treatment of PCOS.
Do you have to severely restrict carbohydrates to improve insulin resistance? Not necessarily.
While going low carb has been shown to improve fertility and hormonal function in this 2021 systematic review, the majority of the studies were 3-6 months in length with only 1 study lasting a full year. To go even further, the Keto diet specifically is a very strict low carbohydrate diet, restricting carbohydrates to less than 50g per day. This diet has been shown to improve blood sugar, insulin resistance, and hormonal balance in PCOS in this 2020 study. However, this study is also only 12 weeks in length and doesn't assess for long-term safety of the diet.
Keto diets may have consequences on our long term thyroid health, potentially putting us in a hypothyroid state, gut health due to lack of fiber feeding a healthy microbiome, and hormonal health due to putting the body in a state of stress by restricting carbs.
So what’s the right answer? Realistically, the best diet is going to be one that is sustainable for you. Watching carbohydrate intake should focus on the types of carbohydrates we eat. Here are some general guidelines that can help to improve insulin resistance without excessively cutting carbohydrates.
Sleep plays a major role in the regulation of our blood sugar and insulin levels. Both lack-of and excessive amounts of sleep appear to have negative effects on blood sugar stability, according to this review, with the most ideal sleep length being 7 hours per night. Unfortunately, while the exact cause is unclear, people with PCOS tend to have a more difficult time sleeping.
Causes of slee00 Comments in moderationp disturbances often look different for everyone, so options should be tailored to the individual. Some ways to improve sleep include minimizing screen time before bed, keeping the room dark and cool, keeping a consistent bedtime, and doing breathing exercises or meditation before bed. There are also numerous botanical and nutraceutical remedies that can help promote sleep if needed.
Over-exercising can end up resulting in increased stress on the body, wreaking havoc on our adrenal glands and overall hormonal health. Incorporating various types of exercise, including strength training, HIIT training (short sessions), cardiovascular exercise, yoga and gentle exercises like walking, are all important in creating a sustainable exercise program that works for your lifestyle.
According to this systematic review, 120 minutes per week of "vigorous activity" (meaning enough to break a sweat) helps to improve blood sugar balance in people with PCOS.
The foundational health changes to sleep, nutrition, and exercise are all needed for sustainable change to our blood sugar regulation. Sometimes, though, we need a little extra support boost to get us going. Some supplements that may help to reduce blood sugar and improve insulin resistance include berberine, inositol, magnesium, and chromium.
References:
1. Shang Y, Zhou H, He R, Lu W. Dietary Modification for Reproductive Health in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021;12:735954. Published 2021 Nov 1. doi:10.3389/fendo.2021.735954
2. Paoli A, Mancin L, Giacona MC, Bianco A, Caprio M. Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. J Transl Med. 2020;18(1):104. Published 2020 Feb 27. doi:10.1186/s12967-020-02277-0
3. Kose E, Guzel O, Demir K, Arslan N. Changes of thyroid hormonal status in patients receiving ketogenic diet due to intractable epilepsy. J Pediatr Endocrinol Metab. 2017;30(4):411-416. doi:10.1515/jpem-2016-0281
4. Colberg SR, Zarrabi L, Bennington L, et al. Postprandial walking is better for lowering the glycemic effect of dinner than pre-dinner exercise in type 2 diabetic individuals. J Am Med Dir Assoc. 2009;10(6):394-397. doi:10.1016/j.jamda.2009.03.015
5. Smiley A, King D, Bidulescu A. The Association between Sleep Duration and Metabolic Syndrome: The NHANES 2013/2014. Nutrients. 2019;11(11):2582. Published 2019 Oct 26. doi:10.3390/nu11112582
6. Fernandez RC, Moore VM, Van Ryswyk EM, et al. Sleep disturbances in women with polycystic ovary syndrome: prevalence, pathophysiology, impact and management strategies. Nat Sci Sleep. 2018;10:45-64. Published 2018 Feb 1. doi:10.2147/NSS.S127475
7. Mastorakos G, Pavlatou M, Diamanti-Kandarakis E, Chrousos GP. Exercise and the stress system. Hormones (Athens). 2005;4(2):73-89.
8. Patten RK, Boyle RA, Moholdt T, et al. Exercise Interventions in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Physiol. 2020;11:606. Published 2020 Jul 7. doi:10.3389/fphys.2020.00606
9. Li MF, Zhou XM, Li XL. The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid Based Complement Alternat Med. 2018;2018:2532935. Published 2018 Nov 14. doi:10.1155/2018/2532935
10. Unfer V, Nestler JE, Kamenov ZA, Prapas N, Facchinetti F. Effects of Inositol(s) in Women with PCOS: A Systematic Review of Randomized Controlled Trials. Int J Endocrinol. 2016;2016:1849162. doi:10.1155/2016/1849162
11. Rodríguez-Morán M, Guerrero-Romero F. Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects: a randomized double-blind controlled trial. Diabetes Care. 2003;26(4):1147-1152. doi:10.2337/diacare.26.4.1147
12. A scientific review: the role of chromium in insulin resistance. Diabetes Educ. 2004;Suppl:2-14.
Located within: Blog.
Have a question or need to schedule an office visit?
Please fill out the form below or call 480.771.4422.
have you seen us?

8952 E Desert Cove Ave, Ste 114. Scottsdale, AZ 85260
© 2026 Natural Kid Doc, Dr. Kiera Smialek ND, FABNP
all rights reserved. privacy policy